Several other factors are exacerbating the shortage:
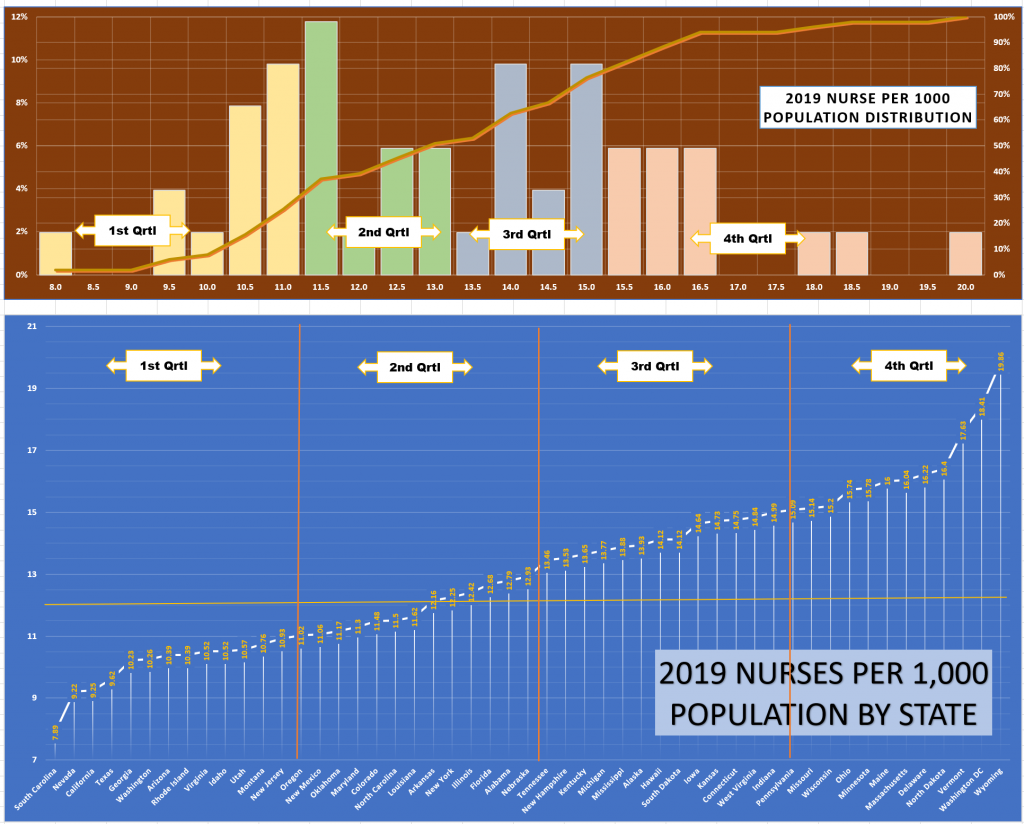
- Location: Statewide nursing shortage estimates are all over the place, with some states projected to have a large shortage (CA >200K by 2030) and some to avoid all together (“if” current ratios of registered nurses per 1,000 inhabitants remain!)
- Rural communities: absorb greater impacts from the nursing shortage than metropolitan areas. About 1 in 6 registered nurses live in rural areas, where they serve more than 50 million Americans.
- Lack of teaching staff: nurses need to be taught by other nurses. But the faculty is also retiring, leaving nursing schools without a strong pipeline of educators to take their place. The 2020 AACN survey found that more than 80,000 qualified applicants to nursing schools were rejected due to a lack of qualified faculty, classroom space, and budget constraints. As a result, fewer nursing graduates will enter the workforce.
- Work Morale: The elevated stress levels of nurses today are due to more than the pandemic, more than the need to make urgent, life-altering decisions, and more than working long hours. It is all of these things and more, combined, that weigh on the shoulders of many registered nurses.
- Misguided budget plans – based on HPPD calculations have led many health centers to cut staffing levels or delay hiring, leaving a significant imbalance in workloads for the remaining nursing staff.
- The Pandemic: Created a need to move nurses out of their typical care roles into intensive care covid units and to lay off others from traditional procedure areas. Both contribute to increases in nursing retirement.
- Some are moving to greener pastures: the private sector (pharmaceutical, biotech, etc.) and the advanced practice clinical sector. The average nurse practitioner earns more than $100k, while the average nursing school assistant professor earns $75k